Guys, What Happened Last Night?
Alcohol: From the Fun Memories to the Dark Blackouts
Come to think of it, alcohol is a very unusual thing. It is the reason for some of your best memories, some of your worst ones or no memories at all whatsoever! How can the very same substance induce the whole spectrum reactions? It is most bizzare.
As a brand new fresher in whichever university, it Is likely many of its planned events will be have a common denominator – Alcohol. The chances are you would make your first friends and memories of your little adult life centred around a drinking game, a night out in the club or a dinner at the pub. You will laugh at and tease your friends’ antics when they do silly things #underinfluence and for some mysterious reason, that may deepen your friendship bond. It is no secret a few drinks can get you less inhibited and naturally makes it easier for you to rock out those moves on the dance floor and become more talkative, full of life and funny!
Alcohol and Hormones
The answers as to why alcohol alters you brain function largely be boils does to its effects on your brain’s chemical messengers or ‘neurotransmitters’. It is thought that alcohol increases the levels of GABA in the brain. GABA is an ‘inhibitory’ chemical messenger that can cause your heart rate and blood pressure to drop and ultimately helps you feel more relaxed. Alcohol also ramps of the levels of dopamine, the ‘happy hormone,’ making sure you get pleasure out of the G&T you poured yourself. Another hormone which alcohol raises the concentration of is noradrenaline, ‘the fight or flight hormone’. It increases your excitement, makes you more impulsive and less afraid – and then you end up doing silly and funny and make some good old memories out of it. However, it is also the reason why, that if the situation took a different turn, things could go downhill and get dangerous very fast. As a doctor, I mostly see the sad horrors alcohol can lead to.
That shift on New Years Eve in the Emergency Department (ED)
I was working New Year’s Eve in ED and you almost definitely expect alcohol associated nuisance. Most of them are a bit of a laugh – they come in drunk, you babysit them in ED for a bit and hook them up to a bag of intravenous fluids – they sober up, they walk out, THE END. But there was one patient that night who I wouldn’t forget. She was a young 30 something year old lady whose little blurb on our digital whiteboard read “Fall whilst drunk, head injury”. She was my next patient to see and a pretty common story for a New Year’s Eve night. I checked the CT scan of her head which did not show any bleed inside the brain or skull vault which means she was most likely all clear. I got ready to call her in, listen to the events which led up to her turning up at A&E and then hopefully discharge her as her blood tests and scans were fine. However, when I went to see her, my jaw dropped….
She had blood smeared all over her face. She had blood dried in the thick locks of her hair it wouldn’t come out. The internal scan obviously couldn’t pick up the extent of her external bleeds and soft tissue injuries on her face. Our nurse was trying to clean the blood off, but it was no easy task. I asked her how she got injured, but she couldn’t say much. She didn’t remember. She was an intelligent girl who worked in finance but that night she couldn’t give me anything on what happened. Nothing at all. The nurse and I quietly worked through with cleaning the wound and what emerged was unreal. She had so badly lacerated her face, there was a long deep cut from her far edge eyebrows round to front of her cheek. I held up the pieces of her face together and I could tell she was very beautiful. However, her lacerations were so complex and way above my junior doctor in ED competency level I referred her to Maxillofacial surgeons. I still have my fingers and toes crossed and hope they were able to restore what was once before.
In that given moment, I passed my off her memory impairment as related to intoxication. We have all know how common it is and my main priority initially was to control her bleeding and to fix her facial cuts. It’s only later I appreciated just how dangerous this “I don’t remember” is particularly when you are inflicted with a serious injury like that. It’s all well and good, someone not remembering that funny thing they said, or that silly dace they did whilst drunk, but ending up with your face in pieces was a big deal not to remember. What if that lady didn’t fall because of lack of coordination but was pushed and harmed and she “didn’t remember?”
Alcohol induced blackouts
An alcohol induced blackout refers to alcohol induced memory loss without any loss of consciousness. So essentially, in a blackout you are not flat out passed out unconscious on the floor – you are still able to walk, talk and hold a conversation but you just have no memory of doing it. Know of anyone who woke up in a friend’s bedroom or other stranger places and have no recollection of how they got there? Yup, that’s a blackout.
So, if you aren’t passed out or unconscious, why does your memory blackout? To understand how alcohol impacts your memories in this way, let me start with what memory is in the first place – the basics of memory at least because I promise there is so much more to memory than we think there is!
First let me start with the different types of memory systems:
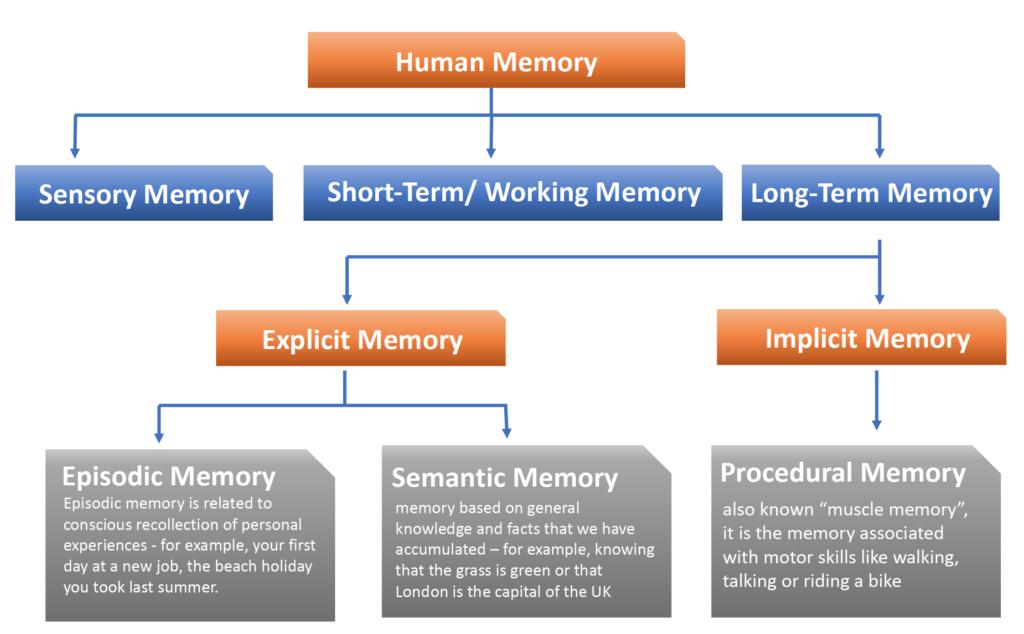
.It is our episodic memory system that is primarily affected by alcohol. Episodic memory is our ability to remember events and life experiences including the time, place and context in which it occurred. Contextual information includes the environment in which the memory occurred, the state of mind (high, low, on drugs, not on drugs) or mood (happy, sad, scared) the individual was in. This context-based information is a prerequisite for episodic memory.
Once we know why type of memory alcohol affects the most, we now need to understand how this memory is formed or coded in our brain.
.Memory, in its full entity consists of three components or stages:
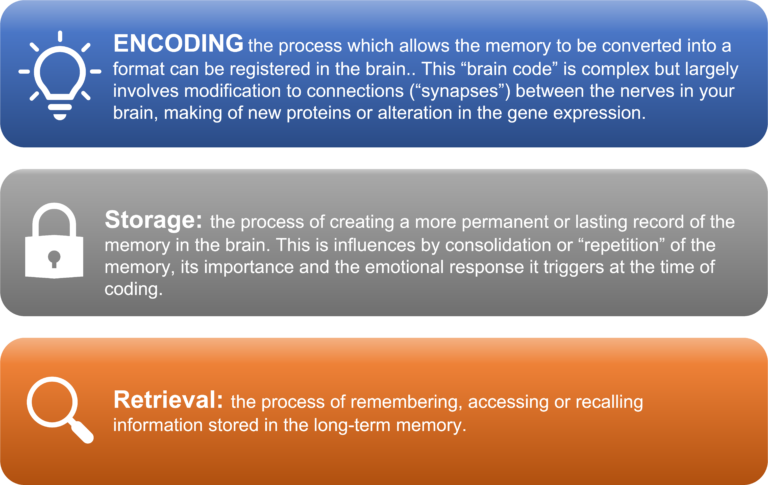
The process in which memory is processed through these different stages can be summarised by the memory model proposed by Atkinson and Shiffrin (1968)- granted big words which daunted me as well when I was doing my cognitive neuroscience degree at Cambridge but it’s a simple linear process really.
.It flows like this:
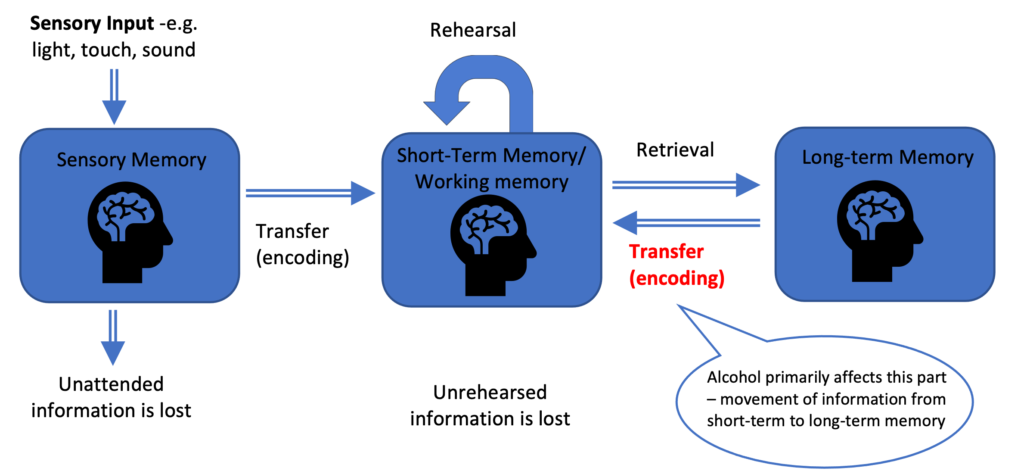
.Sensory information, like a motion picture (visual) or music (sound) is transduced by the appropriate sensory receptors (e.g. rods and cones in the eyes) to information that can be processed by the nervous system. This is stored temporarily in the sensory memory and then transferred to the short term-memory. For example, a telephone number you just hear is modified by the receptors in your ears to a neural code which gets encoded in the short-term memory so you can dial that number there and then and contact the person you wish to contact. If you don’t keep rehearsing that same number, you would forget it and wouldn’t be able to recall it later. But if you keep rehearsing that string of numbers, your ability to recall it further down the line is greatly enhances. The more times you rehearse it the more likely you are to encode it into your long-term memory and remember it the next day.
Alcohol affects all stages of memory processing, but the stage which appears to be disproportionately affected is the transfer of information from short-term to long-term memory. Individuals are who are intoxicated can recall information immediately after it is presented to them and can even hold it in their short-term memory to sustain an apparently normal (ish) conversation. However, as the information is not transferred/encoded in the long-term memory, there is no recollection of it the next day.
Alcohol induced memory loss or ‘amnesia” can be complete (en bloc) or partial (fragmentary). In a complete blackout, memory cannot be recalled no matter what the circumstance. Fragmentary blackouts are more common, and recall be aided by cueing. For example, reminding the person of the location, or the people, or events surrounding the missing memory in question can help aid recall. This may be due alcohol’s effect on encoding can disrupt the processing of contextual information essential for episodic memory. Cueing individuals with the context during which the memory was formed, can five access the memory which was poorly encoded.
You don’t need to be an alcoholic to have a blackouts
You don’t need to be an alcoholic to have blackouts. You don’t even need to have consumed too much alcohol to have a blackout. In fact, many of those who have had blackouts reminisce that they have had much more alcohol previously without having a blackout. Blackouts occur, if you drink too much, TOO FAST. It is the rapid rise of blood alcohol concentration which is most closely associated with alcohol induced blackouts. So chugging down liquor on an empty stomach, bad idea. The social and environmental context also influences your likelihood of having a blackout. Imagine a first year college campus where drinking is not just tolerated but encouraged (Downnnn itttt!!, remember?). Now, compare this population to a middle-aged married adults with young toddlers – we know which group of people are more likely to have a black-outs.
Alcohol induced blackout is not necessarily a sign of brain dysfunction and there are no recognised baseline memory differences in those who experience blackouts versus those who do not. Most people “grow out” of these problem-drinking related blackouts as they graduate, getting married or successfully entering adult working life., For some those, chronic alcoholism and chronic blackouts is a red flag and need treatment. In severe cases, it can result in complete and permanent loss in the ability to make memories. Keep an eye out for my blog post ‘How Can Alcohol Make You Lose Your Memory…..Forever” to learn more!
Resources:
- My lectures on memory during my BA Cognitive Neuroscience degree at Cambridge
- White AM. What happened? alcohol, memory blackouts, and the brain. Alcohol Res Health. 2003;27(2):186.
- Lee H, Roh S, Kim D. Alcohol-Induced Blackout. International Journal of Environmental Research and Public Health. 2009;6(11):2783-2792.